Stephen H Tsang, MD, PhD
On the web
Overview
Stephen H. Tsang, M.D, Ph.D. is an acclaimed clinical geneticist in the care of individuals with retinal degenerations. He has been culturing stem cells since 1992 and created the first mouse model for a recessive form of retinitis pigmentosa (RP) by applying genome engineering to stem cell technology in 1995. He successfully treated preclinical models of Pde6a, Pde6b, Mfrp, Rho, Cngb1 and autosomal recessive bestrophin retinopathies.
He has expertise in designing and testing genome engineering strategies in pre-clinical models, developing patient-specific knock-in models, generating of patient cell lines and providing care to patients with a precision medicine approach. He is also leading efforts in FDA trials for gene therapies, including PDE6A, RAB geranylgeranyl transferase, RPGR, CNGB3, CNGA3 and ABCA4 retinopathies.
He wrote 3 books: “Precision Medicine, CRISPR, and Genome Engineering: Moving from Association to Biology and Therapeutics" and “Stem Cell Biology and Regenerative Medicine in Ophthalmology”, Springer Press, NY; and “CRISPR Genome Surgery in Stem Cells and Disease Tissues”, Elsevier Inc. He is an elected member of several honorary societies including the American Society for Clinical Investigation, Alcon Research Institute and American Ophthalmological Society. He is consistently named to various NIH study sections (DPVS standing member 2014-8 and PED2 2022-6) and other review committees; Alcon Research Institute Grant Review Committee (2022-27), Scientific Advisory Panel - Research to Prevent Blindness (RPB, 2019-29), Chair of American Ophthalmological Society Thesis Review Committee (2022-2023). Many of his publications are in widely-read general interest journals such as Science, NEJM, Lancet, Cell Stem Cell, Nature Genetics, and Journal of Clinical Investigation, which attests to the broad impact that his work has had.
Dr. Tsang received a resident teaching award in 2008 and was the Columbia Ophthalmology Basic Science Course Director (2006-2018).
Dr. Tsang graduated from Johns Hopkins University, where he began his medical genetics training under the tutelage of Professor Victor A. McKusick. He received his M.D. and Ph.D. degrees from the NIH-National Institute of General Medical Sciences Medical Scientist Training Program (MSTP) at Columbia University. Dr. Tsang then completed his residency at Jules Stein Eye Institute/UCLA, followed by studies with Professors Alan C. Bird and Graham E. Holder on improving the care of individuals with macular degenerations.
Areas of Expertise / Conditions Treated
- Adult Genetics
- Applied Eye Genetics
- Clinical Genetics
- Clinical Molecular Genetics
- Diabetic Retinopathy
- Electrophysiology
- Genetic Disorder
- Genetic Disorders
- Genetic Testing
- Hereditary Retinal Degeneration
- Macular Degeneration
- Marfan Syndrome
- Molecular Biology
- Molecular Medicine
- Pediatric Genetics
- Precision Medicine
- Retina Degeneration
- Retina Disorder
- Retinal Bleeding
- Retinal Disease
- Retinal Disorders
- Retinal Vascular Disorders
- Retinitis pigmentosa
- Retinopathy
- Skin Pigmentation Disorder
- Stem Cell Transplantation
- Vitreoretinal Disorder
Academic Appointments
- Laszlo Z. Bito Professor of Ophthalmology, and Pathology and Cell Biology
Administrative Titles
- Course co-director, BMENE6510 Stem Cells, Genome Engineering and Regenerative Medicine
Hospital Affiliations
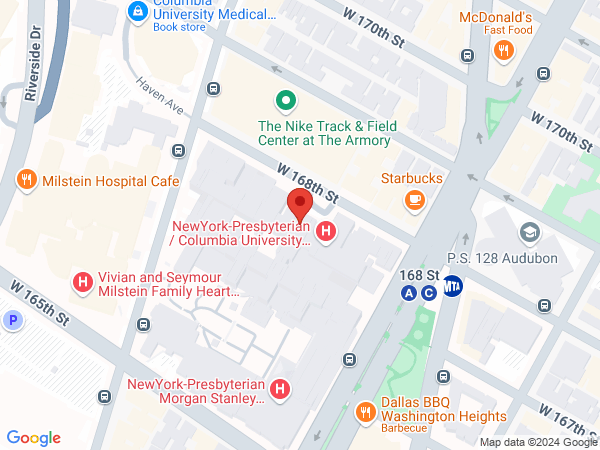
- NewYork-Presbyterian / Columbia University Irving Medical Center
Languages
- Cantonese
Gender
- Male
Schedule an Appointment
Phone Appointments
Connect Patient Portal
For existing patients, login to make an appointment, view documentation or contact your care provider.
Location(s)
Insurance Accepted
Aetna
Cigna
Emblem/GHI
Emblem/HIP
Empire Blue Cross/Blue Shield
Fidelis Care
Local 1199
MagnaCare (National)
Medicare
Multiplan
UnitedHealthcare
WellCare
World Trade Center Health Plan
Credentials & Experience
Education & Training
- Columbia University College of Physicians and Surgeons
- Internship: New York Hospital Queens
- Residency: UCLA - Jules Stein Eye Institute
- Fellowship: Moorfields Eye Hospital, London
Committees, Societies, Councils
Consultant, Cellular Tissue and Gene Therapies Advisory Committee (CTGTAC) at the Center for Biologics Evaluation and Research (CBER),{2020-4 and 2011-9}
NIH DPVS Study Section {2014-8}
American Society for Clinical Investigation
Macular Society
Board Certifications
- Ophthalmology
Honors & Awards
Named Lectureships
- 2020: Keynote Speaker, Symposium on Retinal Degeneration, Universidad Católica de Valencia
- 2015: ARVO 2015 Annual Meeting Personalized Medicine Invited Speaker in Denver, Colorado
- 2015: Dr. Joginder Nath Ophthalmology Lecturer, West Virginia University School of Medicine
- 2013: Dr. Bradley Straatsma Lecturer, UCLA
- 2010: Keynote Speaker, GTCbio 2nd Annual Ocular Diseases & Drug Discovery Conference
- 2006: Dr. Isaac Bekhor Lecturer, Doheny Eye Institute at University of Southern California
Honors
- 2018: Anton Bank Award, Order of the Sons of Italy in America Grand Lodge of New York
- 2018: Young Investigators Award Recipient. Macula Society
- 2017: American Academy of Ophthalmology Achievement Award Recipient. (November 11-14)
- 2016: Elected to American Society for Clinical Investigation
- 2015: Elected to the American Ophthalmological Society
- 2014: Foundation Fighting Blindness Visionary Award Recipient and “Banking on a Cure” Honoree
- 2013, 5, 6: Elected by peers for inclusion in Best Doctors in America®
- 2013: Dr. Paul Stringer Memorial Lectureship, McMaster University
- 2012: ARVO (Association for Research in Vision and Ophthalmology)/Pfizer Carl Camras Translational Research Award
- 2012: ARVO/Genentech Translational AMD Research Award
- 2008: Resident Teaching Award, Columbia University
- 2008: “America’s Top Ophthalmologists,” Consumers’ Research Council of America
- 2008–Present: Elected to Macula Society for Retinal Physicians
- 2007: Charles E. Culpeper Prize in Translational Research
- 2006: ARVO/Alcon Early Career Clinician Scientist Award
- 2005: Becker-RPB-AUPO Award
- 2004: Dennis W. Jahnigen Career Award, American Geriatrics Society
- 2003: Joel Hoffmann Scholar, Columbia University
- 2003: Nesburn Resident Award
- 2003: RPB-Association of University Professors in Ophthalmology Resident
Awards
- 2003: Burroughs Welcome Fund Career Award in Biomedical Sciences
- 2002: Jules Stein Eye Institute Resident Award
- 2000: RPB-Association of University Professors in Ophthalmology Resident Award
- 2000: Jules Stein Eye Institute Research Award
- 1998: John Lattimer Award in Urology, Vagelos College of Physicians and Surgeons, Columbia University
- 1998: Edith McKane Award in Ophthalmology, Vagelos College of Physicians and Surgeons, Columbia University
- 1997: Travel Grant, European Students’ Conference at the Charité in Berlin
- 1997: Best Overall Presentation at Eastern Student Research Forum sponsored by American Medical Association and the University of Miami
- 1997: Dr. Alfred Steiner Award for Best Medical Student Research, Vagelos College of Physicians and Surgeons, Columbia University
- 1996: ACGA Student Award, presented at the ASHG Meeting
- 1996: Dean’s Award for Excellence in Research, Graduate School of Arts & Sciences, Columbia University
- 1995: ARVO/National Eye Institute Travel Fellowship Grant for the ARVO Meeting
- 1995: Certificate of Award, SCBA, Tristate Chapter
- 1989: Student Activities Award, The Johns Hopkins University
- 1989: Graduate with Departmental Honors, The Johns Hopkins University
- 1988–1989: Dean’s List, The Johns Hopkins University
- 1988–1989: Alpha Epsilon Delta, National Premedical Honor Society, Maryland Alpha (Historian 1988–1989)
Research
As a result of his groundbreaking metabolome reprogramming research, Dr. Tsang has earned a reputation as one of the world's foremost authority in therapeutics of neurodegenerative disorders.
Dr. Tsang's genome engineering laboratory is engaged in tackling neurodegenerative disorders by pursuing investigations in three areas, two of which include patient-specific mouse models: probing the role of phosphodiesterase (PDE) signaling in neurodegeneration, developing stem cell-based therapies for photoreceptor degeneration, and correlating the genotypes of various human retinal degenerations with the phenotypes revealed in live metabolic imaging (autofluorescence). Dr. Tsang is also currently focused on genome engineering/CRISRP approaches to reprogramming metabolome in photoreceptor to promote cell survival, which may be broadly applicable to retinal degenerative diseases, regardless of the mutation. While light-adapted normal photoreceptors have a highly anabolic and aerobic (high lactate) metabolism similar to the Warburg effect observed in stem cells, dark-adapted photoreceptors have catabolism (low lactate), high-ATP metabolism similar to neurons. To translate this anabolic therapy to humans (who would rightly reject being maintained in darkness), Dr. Tsang's laboratory is developing “genetic sunglasses” to promote a constant dark-adapted metabolic state in photoreceptor neurons while maintaining a normal light-dark circadian environment.
Research Interests
- Gene therapy
- Genome Surgery
- Neural Degeneration and Repair
- Sensory Physiology
- Stem Cell Biology
Clinical Trials
2014–2019 Global Phase III Trial of Collategene (AMG0001) Critical Limb Ischemia
2014-2017 Phase III Trial of AZD9291 versus Platinum-Based Doublet Chemotherapy Non-Small Cell Lung Cancer
2014–2017 ENDEAR Phase III Trial of ISIS-SMNRx Infantile-Onset Spinal Muscular Atrophy
2014–2016 SUMIT Phase III Trial of Selumetinib (AZD6244: ARRY-142886) (Hyd-Sulfate) Metastatic Uveal Melanoma
2014–2016 STARRS Phase II Trial of Selinexor (KPT-330) Squamous Cell Carcinoma
2014–2016 Phase II Trial of AZD9291Non-Small Cell Lung Cancer
2013–2018 Phase I/II Trial of ASP2215 Treatment-Refractory Acute myeloid Leukemia FLT3 Mutation
2013–2018 Study Title: A Phase 3 Open-Label, Multicenter, Randomized Study of ASP2215 versus Salvage Chemotherapy in Patients with Relapsed or Refractory Acute Myeloid Leukemia (AML)
2013–2018 Phase III Trial of MK-8931m Amnestic Mild Cognitive Impairment in Alzheimer’s Disease
2013–2017 APOLLO Phase III Trial of Patisiran (ALN-TTR02)TTR-mediated Amyloidosis
2013–2015 Phase II Clinical Trial of Revusiran (ALN-TTRsc) TTR-mediated Cardiac Amyloidosis
2015-2018 Phase II Clinical Trial of AAV2-REP1 Choroideremia gene therapy
Selected Publications
H-index 70
Gene therapy and genome surgery in the retina. DiCarlo JE, Mahajan VB, Tsang SH. Journal of Clinical Investigation. 2018 Jun 1;128(6):2177.
Caruso S, Ryu J, Quinn PM, Tsang SH. Precision metabolome reprogramming for imprecision therapeutics in retinitis pigmentosa. Journal of Clinical Investigation. 2020 Jul 13;139239. doi: 10.1172/JCI139239.
Stargardt Juvenile macular Degeneration. Oh JK, Tsang SH. New England Journal of Medicine. 2020 Jun 11 doi: 10.1056/NEJMicm1913388
Tsang S.H., Gouras P., Yamashita C.K., Fisher J., Farber D.B., and Goff SP (1996). Retinal Degeneration in Mice Lacking the γ subunit of cGMP phosphodiesterase. Science 272: 1026.
Tsang S.H., Burns, M. E., Calvert, P. D., Gouras, P., Baylor, D. A., Goff, S. P., and Arshavsky, V. Y. (1998). Role of the Target Enzyme in Deactivation of Photoreceptor G Protein in Vivo. Science. 282, 117.
Tsang S.H., Woodruff, M. L., Chen, C. K., Yamashita, C. Y., Cilluffo, M. C., Rao, A. L., Farber, D. B., and Fain, G. L. (2006). Modulation of phosphodiesterase6 turnoff during background illumination in mouse rod photoreceptors J Neurosci 26, 4472.
Wert KJ, Mahajan VB, Zhang L, Yan Y, Li Y, Tosi J, Hsu CW, Nagasaki T, Janisch KM, Grant MB, Mahajan M, Bassuk AG, Tsang SH. Neuroretinal hypoxic signaling in a new preclinical murine model for proliferative diabetic retinopathy. Signal Transduct Target Ther. 2016;1. pii: 16005. Epub 2016 Apr 22. PubMed PMID: 27195131; PubMed Central PMCID: PMC4868361.
Petersen-Jones S.M., Occelli L.M., Winkler P.A., Lee W., Sparrow J.R., Tsukikawa M., Boye S.L., Chiodo V., Capasso J.E., Becirovic E., Schön C., Seeliger M.W., Levin A.V., Michalakis S., Hauswirth W.W., Tsang S.H. (2018). Patients and animal models of CNGβ1-deficient retinitis pigmentosa support gene augmentation approach. Journal of Clinical Investigation. 128(1):190. doi:10.1172/JCI95161.
1. Li, Y, Tsai, YT, Hsu, CW, Erol, D, Yang, J, Wu, WH, Davis, Richard, Egli, Dieter, TSANG, STEPHEN H. Long-term safety and efficacy of human induced pluripotent stem cell (iPS) grafts in a preclinical model of retinitis pigmentosa. Molecular Medicine18: 1312. Cited 55 times.
Contribution: This high-impact study used a preclinical model for retinitis pigmentosa (RP) to provide the first evidence for human iPS-cell-mediated recovery of visual function. Therefore, this research provided critical feasibility data for therapies using autologous iPS-cell transplantation to treat retinal degenerations in humans. This study is also one of the first to provide strong in vivo preclinical evidence that this potential cell therapy does not induce tumor formation. This discovery was featured in numerous news outlets - including a Medscape Medical News article (1/7/13), and in two Columbia University Medical Center press releases (10/1/12 and 12/20/12).
2. Wert, K.J., Sancho-Pelluz, J., Davis, R.J., Nishina, P.M., and TSANG, S.H. Gene Therapy Provides Long-term Visual Function in a Pre-clinical Model of Retinitis Pigmentosa. (2013) Human Molecular Genetics. 22:558. Cited 18 times.
Contribution: This manuscript is unique in the field of gene therapy in that it demonstrates stable, sustained rescue - both functional and structural. These strong feasibility data provide a solid foundation for moving forward with gene-therapy in patients with a specific genetic form of retinitis pigmentosa (RP). In fact, we are currently recruiting patients for our upcoming gene-therapy trial, "Bringing Gene Supplementation Therapy for PDE6-associated Retinopathies into Clinical Practice"
3. Li Y, Wu W-H, Hsu C-W, Nguyen H-V, Tsai Y-T, Nagasaki T, Maumenee IH, Yannuzzi LA, Hoang QV, Hua H, Egli D, TSANG, S.H. Gene therapy in patient-specific stem cell lines and a preclinical model of retinitis pigmentosa with membrane frizzled-related protein (MFRP) defects. (2014) Molecular Therapy. 2014 Sep;22(9):1688. Cited 15 times.
Contribution: This is the first demonstration that patient-specific induced pluripotent stem (iPS) cells can be used to model a disease phenotype, and study its etiology. This is also the first report of human iPS-derived cells being successfully used as a recipient for viral gene therapy.
4. Yang J, Li Y, Chan L, Tsai YT, Wu WH, Nguyen HV, Hsu CW, Li X, Brown LM, Egli D, Sparrow JR, TSANG, S.H. (2014) Validation of genome-wide association study (GWAS)-identified disease risk alleles with patient-specific stem cell lines. Human Molecular Genetics. Jan 31. PMID: 24497574. Cited 27 times.
Contribution: In vitro models for age-related diseases are invariably based on immortal cells, which are inherently unsuitable for modeling diseases of aging. In this study, we developed a novel human stem-cell-based model for age-related macular degeneration (AMD), an ocular disease with high incidence. We then used these cells to determine the function of two important, but poorly understood AMD risk factors. This is the first demonstration that patient-specific induced pluripotent stem (iPS) cells can be used to model a late onset disease phenotype, and study its etiology.
5. Koch SF, Tsai YT, Duong JK, Wu WH, Hsu CW, Wu WP, Bonet-Ponce L, Lin CS, TSANG SH. (2) Halting progressive neurodegeneration in advanced retinitis pigmentosa. 2015. Journal of Clinical Investigation. 2015 Sep;125(9):3704. doi: 10.1172/JCI82462. Epub 2015 Aug 24. PMID:26301813. Cited 5 times.
Koch SF, Duong JK, Hsu CW, Tsai YT, Lin CS, Wahl-Schott CA, Tsang SH. Genetic rescue models refute nonautonomous rod cell death in retinitis pigmentosa. Proc Natl Acad Sci U S A. 2017 May 16;114(20):5259.
Contribution: Recent follow-up studies to the human RPE65 gene therapy trials demonstrated that the interventions failed to halt or even slow photoreceptor degeneration. As a means to explain this treatment failure, it was suggested that the diseased photoreceptors had reached a "point-of-no-return." In this report, we tested this hypothesis in an RP mouse model, using a novel driver to deliver therapy to all rod photoreceptors at early, mid, and late disease stages. In these optimally treated retinas, not only was function rescued, but photoreceptor degeneration was also halted. Critically, we demonstrated significant sustained rescue, even at the late disease stage.
6. Wu WH, Tsai YT, Justus S, Lee TT, Zhang L, Lin CS, Bassuk AG, Mahajan VB, TSANG SH. CRISPR Repair Reveals Causative Mutation in a Preclinical Model of Retinitis Pigmentosa. Molecular Therapy 2016 Aug;24(8):1388. doi: 10.1038/mt.2016.107. Epub 2016 May 20. PMID:27203441. New publication (May 20), no citations yet.
Contribution: In the current era of next-generation sequencing, copious genetic variants are identified. This report illustrates how CRISPR can be used to validate sequence variants, distinguish between their pathogenicity, and elucidate disease pathophysiology. We applied CRISPR/Cas9 to resolve a century-long debate on the molecular origins of the Pde6brd1/Pde6brd1 (Rd1) mouse., Rd1 mice express two mutations - a murine leukemia virus (Xmv-28) insertion and a nonsense mutation (C to A transversion) in codon 347 - that still remain controversial. We sought to determine whether one or both of these mutations engenders the fast-progressing retinal deterioration typical of Rd1 mice.
7. Moshfegh Y, Velez G, Li Y, Bassuk AG, Mahajan VB, TSANG SH. BESTROPHIN1 mutations cause defective chloride conductance in patient stem cell-derived RPE. Hum Mol Genet. 2016 May 18. pii: ddw126. PMID: 27193166. New publication (May 18), no citations yet.
Contribution: Mutations in the BEST1 gene are clearly linked to eye disease in human RPE, including Best vitelliform macular dystrophy. The mechanism linking mutations in the gene to eye pathology is unknown, and the question of whether BEST1 is a bona fide chloride channel has been remaining in the field. In this report we show that BEST1 encodes a predicted transmembrane anion channel that is calcium-activated and highly permeable to chloride ions. We have taken advantage of iPSC-RPE cell modeling of BEST1 disease, and developed a new approach for directly measuring chloride currents in live patient RPE with a biosensor.
8. Zhang L, Justus S, Xu Y, Pluchenik T, Hsu CW, Yang J, Duong JK, Lin CS, Jia Y, Bassuk AG, Mahajan VB, TSANG SH. Reprogramming towards anabolism impedes degeneration in a preclinical model of retinitis pigmentosa. Hum Mol Genet. 2016 Aug 11. pii: ddw256. PMID: 27516389. New publication (Aug 11), no citations yet.
Contribution: In RP, outer segment (OS) gets shortening which triggers photoreceptor death is mainly due to the imbalance between anabolic and catabolic processes. OS is shed and regenerated daily, but in disease photoreceptors, the rate of shedding exceeds the rate of renewal, leading to significantly shorter OS, excessive anabolic demands and subsequent death. Augmenting anabolism could theoretically fuel protein and lipid synthesis, thus encouraging OS regenesis. Ablation of Tsc1, a transcriptional inhibitor of the mTOR pathway, preserved the structure and function of diseased rod and cone photoreceptors in a preclinical model of RP.
9. Yang J, Bassuk AG, Merl-Pham J, Hsu CW, Colgan DF, Li X, Au KS, Zhang L, Smemo S, Justus S, Nagahama Y, Grossbach AJ, Howard MA 3rd, Kawasaki H, Feldstein NA, Dobyns WB, Northrup H, Hauck SM, Ueffing M, Mahajan VB, TSANG SH. Catenin delta-1 (CTNND1) phosphorylation controls the mesenchymal to epithelial transition in astrocytic tumors. Hum Mol Genet. 2016 Aug 11. pii: ddw253. PMID:27516388. New publication (Aug 11), no citations yet.
Contribution: The tuberosclerosis complex (TSC) syndrome is due to mutations in the mTOR modulator, TSC, and so likely holds the key to major questions regarding the function of mTOR in humans. A major phenotype of TSC is the development of non-malignant astrocytomas in the brain. Using a comprehensive battery of tests, we show the key feature controlling this phenotype is catenin delta-1 phosphorylation by mTOR signaling Our findings suggest malignant and benign astrocytomas differ in this phosphorylation event. The TSC astrocyte phenotype implies they are trapped in the mesenchyme to epithelium transition, and that mTOR tunes this reversible process.
10. Lijuan Zhang, Jianhai Du, Sally Justus, Chun-Wei Hsu, Luis Bonet-Ponce, Wen-Hsuan Wu, Yi-Ting Tsai , Wei-Pu Wu, Yading Jia, Jimmy K. Duong, Vinit B. Mahajan, Chyuan-Sheng Lin, Shuang Wang, James B. Hurley, STEPHEN H TSANG. Reprogramming Sirtuin 6 attenuates retinal degeneration Journal of Clinical Investigation. 2016;126(12):4659.
Contribution: In healthy photoreceptors, glycolysis is balanced by gluconeogenesis; in degenerating rods, the rate of glycolysis is compromised. In our manuscript, we show that reprogramming rods into a state of perpetual glycolytic flux by knockdown of Sirtuin 6 (Sirt6), a transcriptional repressor, preserved the structure and function of diseased rod and cone photoreceptors in a preclinical model of RP. The vast heterogeneity of RP limits the applicability of gene editing strategies to ameliorating the disease, and developing a therapy that is not gene specific is highly desirable.
For a complete list of publications, please visit PubMed.gov(link is external and opens in a new window)